Defining Mental Compulsions
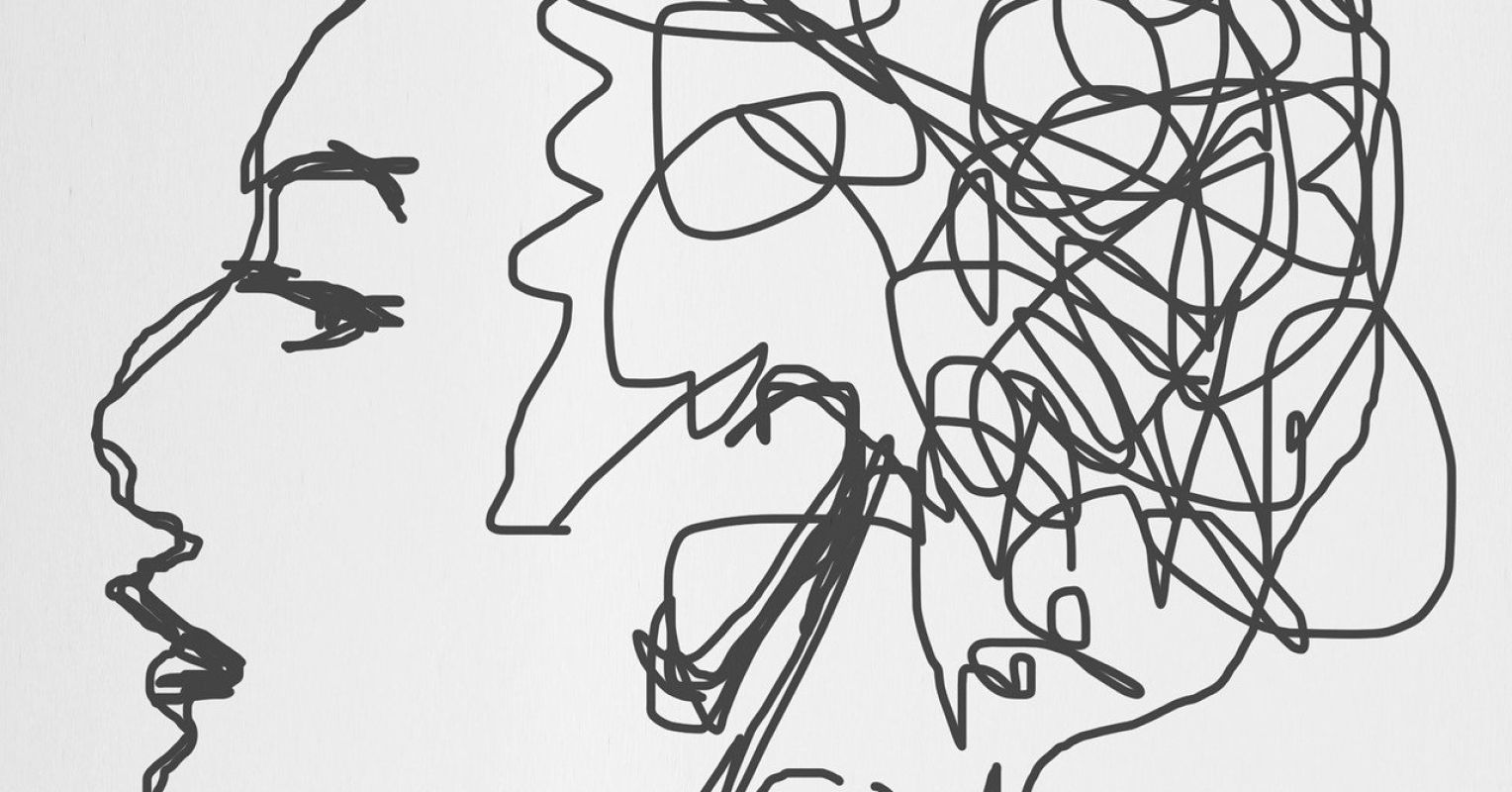
Mental compulsions are repetitive acts played in the mind in response to intrusive, unwanted thoughts. Just like physical compulsions, these mental behaviors are intended to reduce anxiety or prevent a feared outcome. Despite physical and mental compulsions being driven by the same motives, mental compulsions are more covert and can be very subtle, oftentimes tricking the sufferer into not recognizing them as compulsive behaviors that are negatively reinforcing OCD.
For therapists, mental compulsions can be equally challenging to identify. Here are some common mental compulsions that can be present across all subtypes of OCD. Getting familiar with these examples can equip therapists to more promptly determine if mental compulsions are creating barriers for clients reaching their therapeutic goals.
- Mental Review: A mental review commonly presents as an individual replaying a situation, conversation, or other event in their mind over and over again. Some common reasons one may engage in this compulsion would be to gain more certainty (something that OCD constantly wants!), ensure they did not do or say something “wrong” or “bad,” to prevent a feared outcome from happening, to figure something out, or to feel less anxious about the memory/situation.
- Self-reassurance: Self-reassurance is where an individual provides repeated reassurance in their mind to relieve discomfort and distress. Until relief sets in, this can sound like: “Everything is okay.” “I’m going to be fine.” “I’m safe.” “That bad thing isn’t going to happen.” “I didn’t do something wrong.” “I’m not a bad person.”
- Counting: Counting is often done as a means to satisfy one of OCD’s rules. The individual may have to repeatedly count to a certain number until it feels “just right” or count in a certain way to prevent a feared outcome from occurring.
- Praying, Mantras: Repeating prayers and or mantras in the mind is another common mental compulsion that serves to reduce anxiety. This compulsion can be used to provide relief in the moment or used as a way to “make up for” a perceived possible wrongdoing (not probable or grossly exaggerated).
- Using logic: It can be an initial instinct to try to argue back with or out-logic intrusive thoughts when they pop up in the brain. This can include attempts to disprove thoughts by countering with evidence of why they’re not true or using rational statements in response to these thoughts to quell them. (Hint: Attempts to out-logic OCD are exhausting, as OCD will relentlessly keep responding with: “Okay, but what if X then?”)
- Mental Checking: Mental checking involves the individual continuously checking something over and over again in their mind. Examples include visualizing their exact steps before leaving the house to confirm they locked the door or didn’t leave the stove on. The checking continues until the individual feels some short-term relief and can move on, or in more challenging moments, the mental checking may then lead to physical checking to feel safe or certain in the face of the fear.
While these are some examples, it is important to note that OCD, being the sinister monster that it is, can show up in any way imaginable, and therefore the mental compulsions in response to it have infinite possibilities. OCD’s rules can be relentless and outlandish in some cases, making it incredibly challenging for therapists and clients to guess what the mental act may be.
Tip: Individuals who experience compulsions can have both physical and mental compulsions, just physical compulsions, or just mental compulsions.
Mental Compulsions or Typical Cognitive Processes?
Mental compulsions are repetitive and urgent-feeling mental acts performed directly in response to an intrusive thought, image, or urge. Just because an individual may mentally reassure themselves at times, mentally review a situation they were in, or out-logic a thought, does not mean they necessarily have OCD or that they are engaging in mental compulsions. Defining these mental behaviors as compulsions comes down to their function and role. Some questions to consider in determining the function of these mental behaviors could include:
- Is it done often and repeatedly or was this a one-off occurrence?
- Did it feel like it needed to be done, to prevent something bad? To gain certainty? To feel less distressed?
- Did it feel urgent or could it easily have been left alone?
- Is this taking up marked time each day? Is it functionally impairing?
- Are there other mental acts being done in response to unwanted, intrusive thoughts?
- Does it feel enjoyable? In line with values? (A no response can expose the ego-dystonic nature of OCD.)
Considerations for Addressing Mental Compulsions in Treatment
When beginning to address mental compulsions in therapy sessions with clients, it’s helpful to empower clients to understand that mental compulsions are behaviors and therefore are something that can be changed. Differentiating between thoughts, urges, and images that pop into the brain, completely out of one’s control versus engaging with those thoughts as the behavioral choices one makes to reduce the distress, can begin to increase awareness and equip clients with the skills needed to conquer their OCD for the long-haul. It is often a misconception that mental compulsions are happening to the individual. Providing this education, while validating the difficulty of beginning to observe these habits and reduce them, can support clients in their path to recovery.
Once this understanding is in place, the formula for treating physical and mental compulsions becomes more clear to conceptualize. Compulsions, whether they be mental or physical, are the behaviors that are targeted in exposure and response prevention therapy to begin breaking the OCD cycle. Response prevention strategies, such as starting with delaying compulsions, reducing compulsions, and eventually resisting compulsions, will be applied to all compulsions to stop the reinforcement of the unwanted thoughts and the associated distress. This is a collaborative process and gradually paced to create the most effective outcomes with clients and ensure the changes are sustainable for long-term and successful symptom management.
Conclusion
Understanding mental compulsions is vital in providing effective exposure and response prevention therapy for clients working towards recovery with OCD. Understanding mental compulsions, how and when they are happening, and in response to what triggers, will inform the exposure and response prevention goals and create pathways of healing for clients. Increasing quality of life, engaging in valued activities, gaining precious time back in each day, and ultimately breaking the OCD cycle are just some of the benefits of addressing mental compulsions in OCD treatment.
