Have you ever felt embarrassed or worried after noticing a fishy smell in your genital area? If you’re a woman, that smell usually indicates bacterial vaginosis (BV) and can be treated with antibiotics. A new study suggests that BV is not just a concern for women. It turns out that it’s a sexually transmitted infection (STI) and a woman’s male sexual partners should be treated with antibiotics as well.
Overgrowth of “bad” bacteria.
BV is the single most common diagnosis among women who visit a doctor because of excess fluids (or “discharge”) from the vagina. Those fluids often have the odor of “fish.” BV is not caused by a single type of bacteria, but, rather, by a shift in the balance between “good” and “bad” bacteria in the vagina.
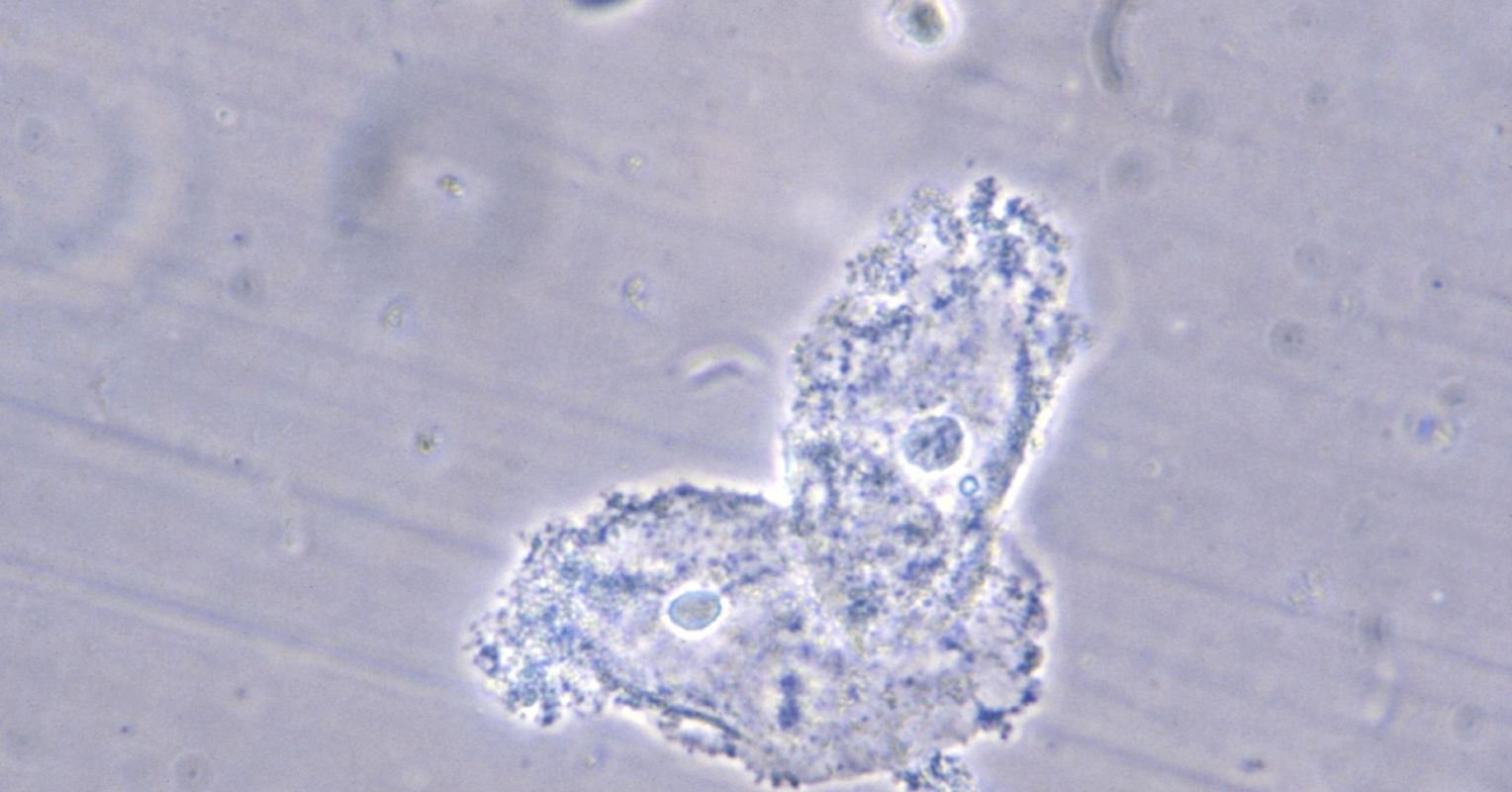
The vagina normally has enough “good” bacteria (Lactobacillus) that keeps the internal environment acidic. In BV, the balance is thrown off with harmful bacteria (like Gardnerella vaginalis) growing in abundance.
These bacteria break down proteins and release amines, the same smelly chemicals responsible for fish odor and certain body smells. As the “bad” bacteria grow more, the environment in the vagina becomes less acidic, which makes the smell of these amines more noticeable, especially after sex or during menstruation.
Is BV Dangerous for My Health?
In addition to being an unwelcome visitor, BV also has habit of coming back again: even after treatment, as many as 60% of women have a recurrence within one year after their last infection.
BV has also been associated with increased risk of HIV, bacterial STIs, and spontaneous abortion and preterm delivery in pregnancy.
Thankfully, treatment for BV is straight-forward: take antibiotics that kill the “bad” bacteria and reset the balance in favor of the good bacteria. The standard treatment approach is to take a pill (metronidazole) or to insert an antibiotic cream directly into the vagina for 5-7 days.
How Did the Study Prove that BV is an STI?
Researchers have believed for many years that BV might be sexually transmitted from men to women. But the proof researchers were looking for was missing. Previous studies did not show that treating men for BV stops women from getting BV.
But researchers in Australia just tried a different approach. In addition to giving men pills to treat the bacteria, they also had them apply a cream to the head of their penis. And this produced a blockbuster result.
The study enrolled 164 adult couples who attested to being monogamous.
If a woman was diagnosed with BV, her male partner was randomly assigned to either receive no treatment (placebo) or a combination of oral metronidazole and a 2% clindamycin cream applied to the penile skin.
The trial was so successful that the ethics committee decided to stop it early. When comparing 81 couples in which the male partner was treated to 83 couples in which the male partner was not treated, the risk of the woman having BV come back again was 63% less.
What Does the New Study Mean for You?
This study confirmed that male partners can transmit bacteria that cause BV to their female partners.
If you’re a woman with vaginal discharge, a fishy smell, and sexual partners who have a penis, make sure those partners get treated with oral antibiotics and a topical cream.
This finding shifts how we think about BV, categorizing it as a sexually transmitted infection. But with this new classification comes both benefits and challenges.
Is There a Problem Labeling BV an STI?
Words shape how we think about diseases. When doctors label an infection “sexually transmitted,” it often triggers moral judgment, fear, and stigma in a way that infections acquired through other routine, healthy activities—breathing, eating, exercising—do not.
People with STIs are often unfairly perceived as ‘dirty’ or ‘reckless,’ while those with the flu or a stomach infection face no such stigma.
How will public perception of BV change now that it’s an STI? History suggests that the shift could be significant.
Consider cervical cancer: Before it was widely known that human papillomavirus (HPV) caused it, cervical cancer was primarily viewed as a random tragedy. Getting it meant you had bad luck. When the HPV vaccine became a standard public health recommendation, people became widely aware that cervical cancer was sexually acquired. The disease itself remained the same, but our understanding of its transmission changed, reshaping public perception.
A similar debate emerged with Mpox (formerly known as monkeypox). During the 2022 outbreak, the overwhelming majority of cases occurred in men who have sex with men, leading to tense discussions about whether to classify Mpox as an STI. Some public health officials hesitated, worried that the label would fuel discrimination and deter broader awareness of the virus. I and others argued that classifying it as an STI was both scientifically accurate and necessary to target interventions effectively.
These debates highlight a central tension in public health: Labeling an infection an STI can focus attention on effective prevention and treatment, but it also invites stigma that can drive people away from seeking care.
The reality is that sex, like eating or breathing or exercising, is a normal health-enhancing activity for humans, and public health officials should be focused on making all activities as free from infection as possible – without shaming the activity itself. No one hesitates to seek treatment for a gastrointestinal infection after dining at a restaurant or a respiratory illness after flying on a plane. Yet, when an infection is linked to sex, shame and silence too often replace open discussion and medical care.
What Should You Do about BV?
If you are in a sexual relationship and one of you has BV, make sure both partners get treated. Keep in mind that not all doctors are up to date on the latest advances, so point them to this article or the original study.
For our society, I hope that this important medical and scientific advance will make us all healthier and not fuel stigma. Classifying BV as an STI presents an opportunity to improve the health of all of us by expanding treatment to men and women and, over time, reducing the adverse health risks associated with BV in women.
